Most people notice it starting small. Bronchitis usually begins with a dry cough that slowly turns productive. The change confuses some. They think it’s a cold stretching out. But mucus production increases daily. The color may shift from clear to yellow or green. Despite the noise, the lungs often remain clear on examination. Chest pain is usually absent. Breathing feels labored but not restricted. The body fights through with rest and fluids, not always needing antibiotics.
Pneumonia often starts abruptly and brings fever, chills, and sharp chest pain
The onset tells a different story. Pneumonia often starts abruptly and brings fever, chills, and sharp chest pain. You don’t ease into it. It hits harder. Patients describe shivering under blankets and feeling short of breath walking across a room. Pain increases while inhaling. Fever climbs fast. Breathing sounds change. Doctors often hear crackles or decreased breath sounds. This isn’t just discomfort—it suggests a deeper infection in the lung tissue.
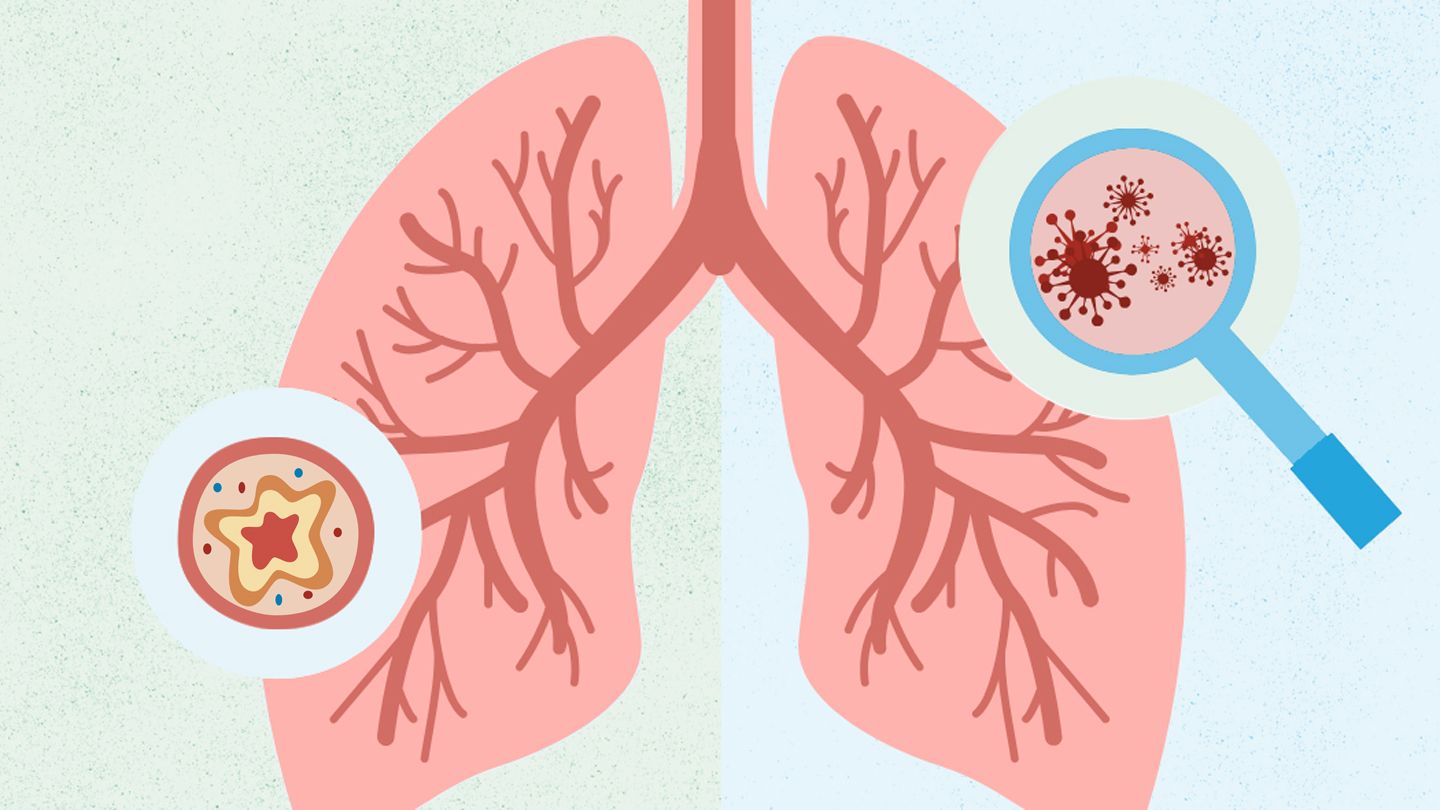
Bronchitis affects the bronchial tubes but spares the actual lung tissue
Understanding the site helps. Bronchitis affects the bronchial tubes but spares the actual lung tissue. These tubes carry air from the windpipe into the lungs. When irritated, they swell and fill with mucus. This causes the classic wheezing sound. But oxygen levels rarely drop. The inflammation stays within the airways. It doesn’t invade lung sacs. This limits the severity. Oxygen exchange continues, even if coughing worsens at night.
Pneumonia fills the alveoli with fluid, reducing oxygen exchange
The process runs deeper in pneumonia. Pneumonia fills the alveoli with fluid, reducing oxygen exchange. These air sacs enable oxygen to enter the bloodstream. Once they’re clogged, breathing becomes a chore. The body tires fast. Pulse oximeters show lower oxygen saturation. Skin may look pale or bluish. It’s not just inflammation—it’s compromise. The lungs can’t keep up. Hospitalization becomes more likely when breathing grows shallow or confused speech appears.
People often mistake bronchitis for a lingering cold
The overlap creates confusion. People often mistake bronchitis for a lingering cold. Runny nose, sore throat, and cough all blur together. A viral infection often triggers bronchitis. It follows a cold but doesn’t resolve as quickly. The cough lingers for weeks. It might be dry or wet. Fever is rare. Fatigue builds slowly. Patients often return to work too soon, worsening symptoms. Recovery takes longer than expected.
Bacterial pneumonia can follow untreated viral bronchitis
Sequence matters. Bacterial pneumonia can follow untreated viral bronchitis. The lungs weaken after long-term irritation. Mucus becomes stagnant, creating ideal conditions for bacteria. Suddenly, symptoms shift. Fever rises. Cough worsens. Breathing grows heavier. This shift signals something new is happening. Doctors repeat imaging or change medications. The transition from viral to bacterial doesn’t always feel distinct, but timing helps guide diagnosis.
Chest X-rays typically appear normal in bronchitis cases
Imaging draws a clear line. Chest X-rays typically appear normal in bronchitis cases. The inflammation doesn’t penetrate deep enough to register. You might hear wheezing or mild crackles, but films remain clear. Doctors diagnose based on symptoms and duration. No shadows appear. This reassures both patient and clinician. But it doesn’t mean it’s comfortable. Bronchitis can still exhaust the body for weeks.
Pneumonia shows up clearly on X-rays, often with visible lung consolidation
The X-ray tells a different story here. Pneumonia shows up clearly on X-rays, often with visible lung consolidation. These white patches signal fluid or pus in lung tissue. Doctors use them to confirm diagnosis and gauge severity. Location matters too. Some cases involve one lobe. Others cover both lungs. Repeat imaging may track progress. In severe pneumonia, these images help determine hospital needs.
Bronchitis tends to improve gradually with supportive care
Time plays a role. Bronchitis tends to improve gradually with supportive care. Rest, fluids, and cough suppressants often help. Antibiotics rarely make a difference unless bacterial. Inhalers may ease wheezing. Most cases resolve in two to three weeks. A lingering cough may continue beyond that. Patience helps more than prescriptions. Doctors reassure rather than intervene aggressively.
Pneumonia may worsen without targeted antibiotics and sometimes oxygen support
Pneumonia requires more. Pneumonia may worsen without targeted antibiotics and sometimes oxygen support. Delay in treatment causes complications. Fluid buildup, lung abscesses, and sepsis may follow. Patients with chronic illness or weak immunity face higher risks. Doctors act faster here. Oral antibiotics may work for mild cases. Intravenous therapy supports severe ones. In elderly patients, symptoms appear vague but progress fast. Hospital admission becomes necessary when home care fails.
Walking pneumonia confuses many because symptoms appear mild but linger long
Labels complicate things. Walking pneumonia confuses many because symptoms appear mild but linger long. It’s often caused by atypical bacteria like Mycoplasma pneumoniae. Fever stays low. Fatigue lasts for weeks. X-rays still show inflammation. Patients don’t always feel very sick. But their energy never returns fully. Cough becomes stubborn. Doctors must explain that mild pneumonia still affects performance.
Bronchitis often causes more upper airway noise than pneumonia
Sound tells part of the story. Bronchitis often causes more upper airway noise than pneumonia. Coughs sound wet and loud. Wheezing is frequent. You hear it even without a stethoscope. Mucus shifts with position. This noise doesn’t equal severity. It means air is still moving. Pneumonia, in contrast, often sounds quieter but signals deeper trouble. Silent lungs may signal consolidation or collapse.
Shortness of breath in pneumonia doesn’t match the exertion level
Breathing changes feel different. Shortness of breath in pneumonia doesn’t match the exertion level. A simple activity like climbing stairs leaves patients winded. This disconnect stands out. The body doesn’t recover easily. Lungs aren’t exchanging gases properly. Even rest doesn’t bring full relief. Doctors check oxygen saturation to confirm. It’s not always visible, but it’s measurable.
A barking cough in bronchitis can persist even after other symptoms disappear
Symptoms don’t leave at the same pace. A barking cough in bronchitis can persist even after other symptoms disappear. It becomes the last part to fade. This frustrates patients. They feel better but still can’t sleep through the night. Cold air or talking triggers spasms. It takes weeks to normalize. Cough syrups may help, but time heals it slowly.
Pneumonia may cause chest pain that worsens with deep breaths or coughing
Pain can be misleading. Pneumonia may cause chest pain that worsens with deep breaths or coughing. This is called pleuritic pain. It comes from inflamed lung lining. Sharp and localized, it doesn’t feel like muscle strain. Patients avoid deep breathing, which worsens oxygen exchange. Pain relief helps, but antibiotics must solve the root. Ignoring this pain delays healing.
Viral bronchitis spreads easily in households and classrooms
Contagion adds pressure. Viral bronchitis spreads easily in households and classrooms. One person’s cold turns into another’s cough. Handwashing and distancing reduce spread. Kids bring it home from school. Siblings share symptoms. Most recover without complications. But some develop asthma-like reactions. Doctors monitor breathing closely, especially in children or the elderly.
Bacterial pneumonia isn’t as contagious but poses higher risk to vulnerable groups
Pneumonia plays by different rules. Bacterial pneumonia isn’t as contagious but poses higher risk to vulnerable groups. Transmission usually needs close contact. But elderly people and those with chronic disease catch it easily. Nursing homes see fast spread. Preventive vaccines help. Annual flu shots and pneumococcal vaccines lower risk. Doctors recommend them for high-risk groups. They don’t eliminate disease but reduce severity.
Some cases of bronchitis resolve without ever needing a doctor visit
Not every case requires medical help. Some cases of bronchitis resolve without ever needing a doctor visit. People rest at home, sip tea, and recover slowly. Over-the-counter meds ease symptoms. If no fever or shortness of breath appears, many wait it out. But symptoms lasting over three weeks need review. A second illness may be hiding behind the first.
Pneumonia often returns in patients who don’t finish their full antibiotic course
Habits affect outcome. Pneumonia often returns in patients who don’t finish their full antibiotic course. Symptoms improve, so pills stop. But bacteria remain. They grow back stronger. Doctors stress completion of medication. Even if you feel fine, the infection may not be gone. Recurrent pneumonia becomes harder to treat. Resistance builds. Trust the prescription timeline.